Breast implants today are safer than ever. Dr. Castor uses FDA-approved options and prioritizes your long-term wellness. Many women struggle with concerns about Tampa Bay breast implant safety, wondering about cancer risks, FDA recalls, and long-term complications that could affect their health and lifestyle.
Tampa Breast Implant Safety – The Key Takeaways
- Modern breast implants are safer than ever, with FDA approval and rigorous testing.
- Rare complications like BIA-ALCL affect fewer than 1 in 3,000 patients with textured implants.
- Saline and silicone implants both have excellent safety profiles when properly maintained.
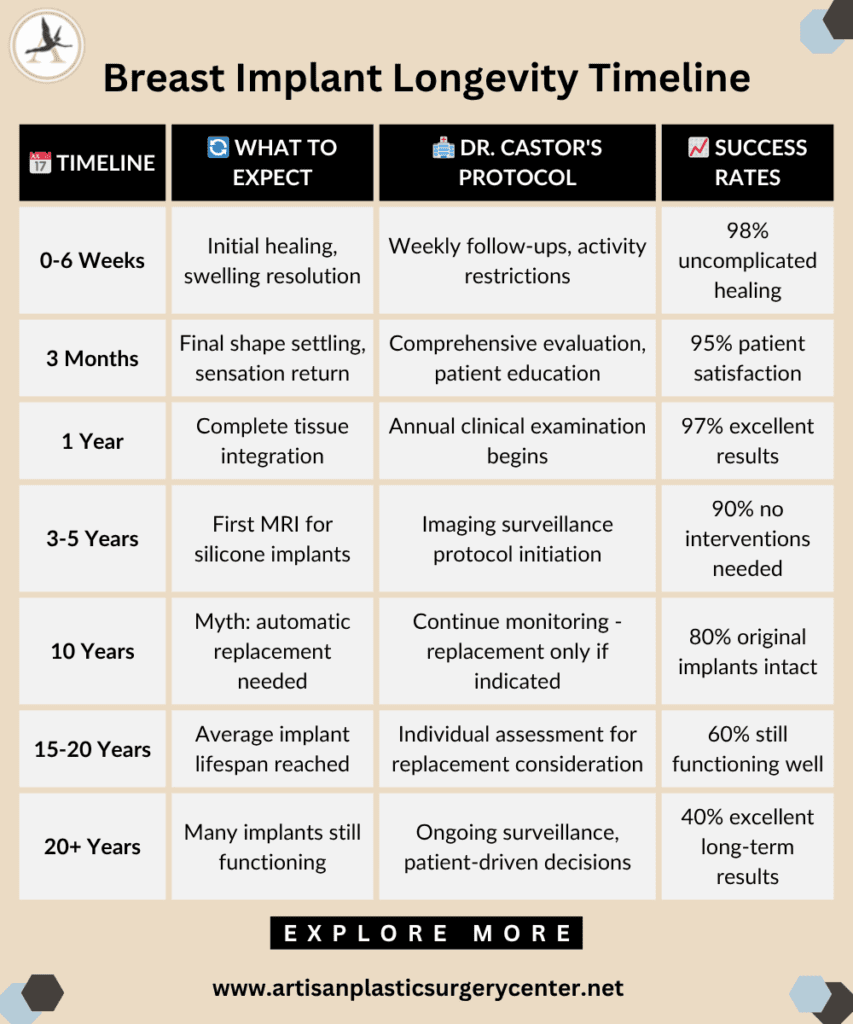
- Most implants don’t require replacement at 10 years – the average lifespan is 15-20 years.
- Regular monitoring and choosing an experienced surgeon minimizes risks significantly.
- Autoimmune conditions don’t automatically disqualify candidates for breast augmentation.
After twenty-one years of practice and thousands of successful breast augmentation procedures at Artisan Aesthetics, I’ve witnessed the evolution of breast implant technology and safety standards firsthand. When I founded my Tampa practice in 2007, my goal was simple: provide patients with honest, comprehensive information about their surgical options while delivering results that exceed expectations.
Today, I want to address the questions that keep my patients awake at night – the real concerns about breast implant safety, risks, and what to expect over the long term. These aren’t just medical statistics to me; they represent real women who trust me with their bodies and their confidence.
Tampa Breast Implant Safety – The Considerations
At Artisan Aesthetics, I provide comprehensive breast surgical procedures with transparent education about implant safety, personalized risk assessment, and evidence-based surgical techniques that prioritize patient well-being over two decades of practice. Learn how to assess safety, surgeon credentials, and aftercare.
What Are the Side Effects of Breast Enlargement Surgery?
Every surgical procedure carries inherent risks, and breast augmentation is no exception. During my years at Watson Clinic in Lakeland and now at Artisan Aesthetics, I’ve seen virtually every possible outcome, both excellent and challenging.
The most common side effects I discuss with patients include temporary swelling, bruising, and discomfort that typically resolve within two to four weeks. More concerning are the persistent side effects that affect roughly 15-20% of patients: changes in nipple sensitivity, either decreased sensation or hypersensitivity, which may be permanent in some cases.
I recently had a patient, Megan, who experienced temporary numbness in her left nipple after her augmentation. During her three-month follow-up, she was concerned this might be permanent. Fortunately, sensation returned gradually over six months, but this illustrates why I spend considerable time discussing these possibilities during consultation.
Scarring is another inevitable side effect, though modern techniques minimize visibility. I use the inframammary approach in about 85% of my cases, creating a small incision in the natural fold beneath the breast. This typically heals to a thin, barely visible line within a year.
What Are the Most Possible Risks of Breast Implant Surgery?
Beyond common side effects, serious risks require careful consideration. Infection occurs in approximately 2-4% of cases, usually within the first few weeks post-surgery. I’ve had to remove implants in three cases over my career due to persistent infection that didn’t respond to antibiotic therapy.
Implant rupture affects roughly 1-2% of patients annually after the first few years. Saline ruptures are immediately obvious – the breast deflates noticeably within hours. Silicone ruptures can be “silent,” detectable only through MRI screening, which is why I recommend MRI surveillance every few years for silicone implant patients.
Capsular contracture is a very frustrating issue for surgeons and patients alike. This occurs when scar tissue around the implant tightens excessively, causing firmness, distortion, or pain. Rates vary from 5-15% depending on multiple factors, including implant type, placement, and individual healing response.
I remember Sandra, a 34-year-old teacher who developed grade III capsular contracture eighteen months after her initial surgery. Despite having beautiful initial results, the contracture required surgical correction with implant replacement and capsule removal. Her second surgery went perfectly, and she’s been thrilled with her results for over five years now.
Is It True That Breast Augmentation Can Cause Cancer?
This question reflects one of the most persistent myths in plastic surgery. Breast implants do not cause breast cancer. Multiple large-scale studies involving hundreds of thousands of women have consistently demonstrated this. In fact, some studies suggest slightly decreased breast cancer rates in augmented women, possibly due to increased surveillance and earlier detection.
However, implants can complicate breast cancer screening. Mammography requires special techniques and additional views, and some breast tissue may be obscured. I always discuss this with patients and ensure they establish care with radiologists experienced in imaging augmented breasts.
The confusion often stems from discussions about BIA-ALCL, which is not breast cancer but a rare form of lymphoma associated with certain textured implants.
What Is the Link Between Lymphoma and Breast Implants?
Breast Implant-Associated Anaplastic Large Cell Lymphoma (BIA-ALCL) represents a legitimate but rare concern that emerged in medical literature around 2011. This is not breast cancer but rather a cancer of the immune system that develops in the scar tissue capsule around certain textured breast implants.
The numbers put this risk in perspective: fewer than 1,000 cases have been reported worldwide among millions of women with breast implants. Most cases occur with heavily textured implants, particularly the Biocell textured surface, which led to the recall of certain Allergan products in 2019.
At Artisan Aesthetics, I stopped using heavily textured implants in 2018, well before the FDA recall, after reviewing emerging data. I now primarily use smooth-surface implants or those with minimal texturing, which have virtually eliminated this risk for my patients.
When detected early, BIA-ALCL has excellent cure rates with implant removal and capsulectomy. This is why I emphasize the importance of reporting any unusual changes, persistent swelling, pain, or masses around implants to your surgeon immediately.
Which Rare Form of Cancer Is Linked with Breast Implants?
BIA-ALCL is currently the only cancer definitively linked to breast implants. This lymphoma typically presents as fluid accumulation around the implant (seroma) occurring months to years after surgery, often accompanied by swelling, pain, or a palpable mass.
Diagnosis requires fluid analysis or tissue biopsy showing characteristic CD30-positive cells. Treatment involves complete implant removal with en bloc capsule excision – essentially removing the implant and all surrounding scar tissue in one piece.
I’ve personally never encountered a case of BIA-ALCL in my practice, largely because I transitioned away from high-risk textured implants early. However, I maintain vigilant surveillance protocols for all my implant patients, regardless of implant type.
What Is Breast Augmentation and Capsular Contracture?
Capsular contracture remains the most common reason for revision surgery in breast augmentation patients. When we place any foreign object in the body, including breast implants, the body naturally forms a protective capsule of scar tissue around it. This is normal. Problems arise when this capsule becomes excessively thick or contracts. We grade contracture severity using the Baker classification:
- Grade I: Soft, natural feel (normal).
- Grade II: Slightly firm but looks normal.
- Grade III: Firm with visible distortion.
- Grade IV: Hard, painful, with significant distortion.
Grades III and IV typically require surgical correction. Risk factors include infection, bleeding, genetic predisposition, and possibly implant surface texture. Interestingly, submuscular placement significantly reduces contracture rates compared to subglandular placement.
One of my most memorable cases involved Maria, a 28-year-old nurse who developed bilateral grade IV contracture just eight months after surgery. Despite perfect surgical technique and no complications during healing, she developed severe contracture requiring complete implant replacement with capsule removal. Her case reinforced my commitment to thorough patient education about this unpredictable complication. Explore more about the signs that breast augmentation might be right for you.
Why Are Textured Breast Implants Being Recalled?
The FDA’s 2019 recall of Allergan’s Biocell textured implants directly resulted from accumulating evidence linking these specific implants to BIA-ALCL. The recall affected roughly 100,000 women in the United States.
Implants with a textured surface were first created to lower the chances of capsular contracture occurring. They were also designed to stop the implants from rotating inside the body. The surface texture theoretically allows tissue ingrowth, creating better implant stability. However, certain aggressive texturing patterns appear to create chronic inflammation that may trigger lymphoma development in susceptible individuals.
The recall specifically targeted Biocell-textured implants due to their association with the highest BIA-ALCL rates. Other textured surfaces remain available, though many surgeons, including myself, have moved toward smooth implants or those with minimal surface texturing.
What Is Breast Implant Surgery, and Is It Safe?
Breast implant surgery, or augmentation mammoplasty, involves placing silicone or saline-filled implants to increase breast size, restore volume, or improve symmetry. The procedure typically takes 60-90 minutes under general anesthesia and can be performed on an outpatient basis.
Breast implants’ safety depends largely on the surgeon’s experience, patient selection, and adherence to established protocols. Board certification by the American Board of Plastic Surgery ensures your surgeon has completed appropriate training and maintains continuing education requirements. My approach emphasizes several safety principles developed over two decades of practice:
- Comprehensive preoperative evaluation, including medical history, physical examination, and baseline mammography for appropriate candidates.
- Meticulous surgical technique with attention to hemostasis, sterile handling of implants, and precise pocket dissection.
- Postoperative monitoring with regular follow-up appointments and patient education about warning signs requiring immediate attention.
Statistical data from the American Society of Plastic Surgeons (ASPS) shows breast augmentation maintains one of the highest patient satisfaction rates among all cosmetic procedures, with over 95% of patients reporting satisfaction with their results.
Are Silicone Breast Implants Safe?
Modern silicone breast implants bear little resemblance to the first-generation devices from the 1960s and 1970s. Today’s fifth-generation implants feature cohesive silicone gel that maintains its shape even if the implant shell is damaged.
The FDA’s extensive review process, culminating in re-approval for general use in 2006, involved rigorous testing and long-term follow-up studies. Data from over 40,000 women followed for ten years demonstrates excellent safety profiles with low complication rates.
Silicone implants offer several advantages, including a more natural feel, especially in thin patients with minimal natural breast tissue. They’re less prone to visible rippling and generally provide superior aesthetic results in primary augmentation.
The main disadvantage involves rupture detection. Silicone implants can rupture without any signs. An MRI scan is required to detect these silent ruptures. This differs from saline implants, where a rupture is easily noticeable. I recommend MRI surveillance every few years for silicone implant patients, beginning three years post-surgery.
What Happens When a Saline Breast Implant Deflates?
Saline implant deflation creates an unmistakable change – the affected breast loses volume dramatically within hours to days. While alarming, this represents no health risk since saline is simply sterile salt water that the body absorbs harmlessly.
I experienced this scenario with Patricia, a 42-year-old mother who called my office panicked because her left breast had “deflated overnight” six years after her original surgery. She came in immediately, and examination confirmed complete saline implant deflation.
Deflation typically results from valve failure or fold fatigue in the implant shell. While inconvenient, it provides an opportunity to assess the implant pocket, address any capsular issues, and potentially upgrade to newer implant technology.
Surgery to replace a deflated saline implant is generally straightforward, often performed through the original incision with minimal additional scarring. The process of replacing an existing implant is generally quicker compared to the initial implant procedure because the pocket or space for the implant has already been created.
Tampa Breast Implant Safety – The Longevity
Can Breast Implants Last 30 Years?
While breast implants aren’t considered lifetime devices, many exceed 20-30 years without problems. The “10-year rule” represents outdated thinking based on earlier implant generations with higher failure rates.
Current data suggests an average implant lifespan of 15-20 years, with many lasting significantly longer. I have patients from my early practice days, nearly twenty years ago, who still have their original implants with excellent results and no complications. Factors affecting implant longevity include:
- Surgical technique and implant handling.
- Implant quality and manufacturing standards.
- Individual patient factors, including activity level.
- Regular monitoring and early detection of problems.
The decision for implant replacement should be based on problems or the patient’s desire for change, not arbitrary timelines.
Do I Have to Get My Implants Replaced After 10 Years?
Absolutely not. The “10-year replacement rule” represents one of the most persistent myths in breast augmentation. This misconception likely originated from early implant warranties and outdated FDA recommendations.
Current medical evidence supports monitoring rather than prophylactic replacement. If implants are functioning well with no complications, replacement surgery introduces unnecessary risks without medical benefit.
I tell patients to think of breast implants like automobiles. With proper maintenance and monitoring, they can last decades. However, like cars, they may eventually require replacement due to wear, damage, or the desire for newer models.
Regular follow-up appointments allow early detection of potential problems when they’re easier to address. I recommend annual clinical examinations and periodic imaging for silicone implants.
Tampa Breast Implant Safety – Choosing the Right Profile Type
Can You Leave Saline Implants in Forever?
Theoretically, yes. Saline implants can remain in place indefinitely if they’re functioning properly and the patient is satisfied with their appearance. Unlike silicone implants, saline deflation is immediately obvious, eliminating concerns about undetected problems. However, several factors may eventually necessitate replacement and concern Tampa breast implant safety:
- Patient’s desire for size or type changes.
- Weight fluctuations affect breast appearance.
- Natural aging changes in breast tissue and skin.
- Implant deflation or other mechanical problems.
- Development of complications like capsular contracture.
The key is ongoing communication with your plastic surgeon and regular monitoring to detect any changes requiring attention. Discover more tips on achieving sustainable weight loss.
Why Is Silicon Used in Electronics and Breast Implants?
Silicone’s unique properties make it ideal for both medical and electronic applications. This biocompatible material doesn’t react with human tissue, maintains stability over decades, and provides excellent barrier properties. In breast implants, medical-grade silicone offers several advantages:
- Durability under mechanical stress.
- Natural feel closely resembling breast tissue.
- Stable chemical composition that doesn’t degrade.
- Tissue compatibility with minimal inflammatory response.
The silicone used in breast implants undergoes rigorous purification and quality control processes far exceeding industrial-grade materials. This ensures biocompatibility and longevity appropriate for permanent medical implantation.
What Are the Safest Breast Implants?
Both saline and silicone profiles demonstrate excellent breast implant safety when manufactured by FDA-approved companies and implanted by qualified surgeons. The most suitable implant relies on the individual’s circumstances and personal preferences.
Saline implants offer several safety advantages:
- Lower cost.
- No need for MRI surveillance.
- Immediate deflation detection.
- Smaller incision size due to post-insertion filling.
Silicone implants provide different benefits:
- Lower rippling rates.
- Stable volume over time.
- Better results in thin patients.
- More natural feel and appearance.
At Artisan Aesthetics, I help patients choose based on their anatomy, lifestyle, and personal preferences rather than promoting one type over another.
Can I Get Breast Implants If I Have an Autoimmune Disease?
Autoimmune conditions don’t automatically disqualify candidates for breast augmentation, but they require careful evaluation and consideration. Each case demands individual assessment considering disease activity, medications, and overall health status. Generally, patients with well-controlled autoimmune diseases can safely undergo breast augmentation. However, certain considerations apply:
- Infection risk may be slightly elevated.
- Disease activity should be stable before surgery.
- Immunosuppressive medications may affect healing.
- Close coordination with treating physicians is essential.
I’ve successfully performed breast augmentation on patients with controlled rheumatoid arthritis, lupus, and other autoimmune conditions. The key is comprehensive preoperative evaluation and ongoing communication between all treating physicians.
![]()
Tampa Breast Implant Safety – FAQs and People Also Asked
How often should I have my implants checked?
Annual clinical examinations with your plastic surgeon, plus an MRI every 2-3 years for silicone implants starting at year three.
Will breast implants affect breastfeeding?
Most women with implants can successfully breastfeed, though milk production may be slightly reduced in some cases.
Can I exercise normally with breast implants?
Yes, after full recovery (6-8 weeks), most activities, including exercise, are unrestricted.
What’s the youngest age for breast implants?
FDA approval is age 18 for saline and 22 for silicone implants, though individual maturity and motivation matter more than age alone.
Do breast implants feel different than natural breasts?
Modern implants, especially silicone, closely mimic the natural breast tissue feel, though some differences may be noticeable.
Are breast implants safe in Tampa Bay?
Yes, breast implants are generally considered safe when performed by a qualified and experienced surgeon in Tampa Bay.
What are the risks associated with breast implants in Tampa Bay?
Some risks of breast implants in Tampa Bay include infection, scarring, and potential implant leakage.
How do I choose a reputable surgeon for breast implants in Tampa Bay?
It is important to research potential surgeons, read reviews, and schedule consultations to ensure you feel comfortable and confident in your choice.
How long is the recovery time for breast implants in Tampa Bay?
Recovery time for breast implants in Tampa Bay can vary, but typically ranges from 1 to 2 weeks before patients can resume normal activities.
Can breast implants in Tampa Bay cause cancer?
There have been rare cases of breast implant-associated anaplastic large cell lymphoma (BIA-ALCL), but the risk is very low and can be minimized by choosing FDA-approved implants.
How long do breast implants last in Tampa Bay?
Breast implants don’t last forever. Most women need to get them replaced or taken out after about 10 to 15 years. This is a normal part of having implants and something to think about before getting them. Your doctor should tell you this during your first visit to discuss breast implants.
Will my insurance cover breast implants in Tampa Bay?
Typically, insurance does not cover elective cosmetic procedures like breast implants, but it is important to check with your provider for specific coverage information.
Can I breastfeed with breast implants in Tampa Bay?
Most women with breast implants in Tampa Bay are still able to breastfeed, but it may be more difficult for some individuals.
What is the difference between saline and silicone breast implants in Tampa Bay?
There are two main kinds of breast implants. The first one has salt water inside, while the second one contains silicone gel. Both types work well, but feel a bit different. Both types have their own set of pros and cons.
Are breast implants in Tampa Bay painful?
Most patients experience some discomfort after surgery, but pain levels can vary and are typically well-managed with medication.
Can breast implants in Tampa Bay affect mammogram results?
Breast implants may impact the accuracy of mammogram results, but specialized techniques can be used to ensure accurate screenings.
What are some signs of implant complications in Tampa Bay?
Signs of implant complications in Tampa Bay may include pain, changes in shape or size, redness, and swelling.
Will I need regular check-ups for my breast implants in Tampa Bay, Florida?
It is recommended to have regular check-ups with your surgeon to ensure the health and stability of your breast implants in Tampa Bay.
Can I exercise after getting breast implants in Tampa Bay?
It is important to follow your surgeon’s post-operative instructions, but most patients can gradually resume exercise after a few weeks.
How much do breast implants cost in Tampa Bay, Florida?
The cost of breast implants in Tampa Bay can vary depending on the surgeon, type of implants, and any additional procedures required, but typically ranges from $3,000 to $10,000.
Tampa Breast Implant Safety – Consultation at Artisan Aesthetics Plastic Surgery & Laser Center in Florida
Tampa breast implant safety continues with advancing technology, improved profiles, and evolving surgical techniques. However, the fundamental principles remain unchanged. Choose a qualified surgeon, understand the risks and benefits, and maintain ongoing surveillance for optimal long-term outcomes.
As a plastic surgeon certified by the medical board, I have worked in this field for more than twenty years. In my view, well-informed patients make the best choices regarding their treatment. At Artisan Aesthetics, my team is committed to providing honest, comprehensive information for all breast procedures.
While delivering exceptional results that enhance your confidence and quality of life. Your safety and satisfaction aren’t just professional obligations. Our commitments define every aspect of our practice. Call us at (813) 971-2000 to schedule your complimentary consultation. Discuss breast implant choices suited to your requirements in detail. Additionally, browse through our patient transformation procedure gallery to see the outcomes.

